
Many actors have recently launched significant new initiatives in the domain of climate change and health. Given this important nexus, we undertook a review of funding patterns from 1985 – 2022, using the NIH RePORTER database for the United States and the Dimensions database globally. This includes an assessment of more than 9 million publicly funded projects across both databases with a collective budget of more than $3 trillion. We estimate that between 1985 and 2022 only 0.26% of research funding awarded by the NIH related to climate change, and only 0.70% of funded projects in the Dimensions database related to climate change and human health. Moreover, we thematically map funding patterns according to four thematic areas: changes in climate, the effects of climate change, health impacts, and interventions and strategies. More funding is needed to better anticipate and prepare for the projected health impacts of climate change.



Climate change is a significant and systemic threat to human health. At COP28 in the United Arab Emirates in December 2023, 124 countries endorsed “the Declaration of Climate and Health” and pledged $ 1 billion in new funding efforts 1 . Such an endorsement may be long overdue, given that the World Health Organization estimates that climate change will cause 250,000 additional deaths per year—or 5 million excess deaths every 20 years—through factors such as increased heat stress, exacerbated malnutrition, or the spread of malaria through new flooding, and at least $ 2–$ 4 billion a year in additional direct healthcare burdens 2 . The total toll from climate change since 2000 will surpass 4 million in 2024 3 , a figure greater than the population of Berlin, Germany or Los Angeles, California. The World Health Organization also reports that 3.6 billion people live in areas extremely vulnerable to climate change impacts, and that the death rate from extreme weather events in vulnerable regions such as low-income countries or small island developing states is 15 times higher than less vulnerable ones over the past decade 2 .
Responses to climate change via investments in mitigation or adaptation also have significant intersections with public health. Shindell and colleagues 4 examine the human health implications of achieving a low-carbon pathway aimed at reducing carbon dioxide emissions by about 180 Gigatons of carbon, and estimated that the resulting decreased air pollution would result in ~153 million fewer premature deaths worldwide. Similar findings showcasing the large health co-benefits from climate action have been confirmed by Pearce and Prehoda 5 , Lelieveld and colleagues 6 , Sovacool and Monyei 7 , and Kharecha and Hansen 8 . Pearce and Parncutt 9 calculate that one future premature death is caused every time 1000 tons of fossilized carbon is burned, concluding that if climate change exceeds a 2 °C temperature change, one billion human lives could be lost by the end of this century 9,10 .
The enormity of these estimations makes climate change one of the most pressing health concerns of the modern era, rivaling or even surpassing that of global pandemics such as COVID-19, which resulted in an estimated 3.4 million excess deaths 11 . Previous evaluations suggest that funding research at the intersection of climate change and human health has been insufficient to meet the challenges of the problem, but funding patterns and research trends continue to evolve rapidly 12,13 suggesting the need for an updated assessment. Moreover, comparison across prior studies is hampered by the lack of a standard definition of how to identify funding or research in climate change and health 14 .
Accordingly, in this Perspective we aim to use a standardized approach to provide a comprehensive assessment of trends in funding from 1985–2022 for research relevant to climate change and human health, in the United States and globally. Our objective is to provide potential funders and practitioners insights into patterns of past and present funding, and a justification for the greater funding needed to minimize the adverse health impacts of continued climate change.
In doing so, we make multiple contributions. First, we move beyond bibliometric assessments of the published literature 15,16,17 to examine research funding patterns. Second, we offer a more complete and recent assessment than earlier studies looking at only non-federal funding 18 , or subsets of NIH funding 19,20 . Instead, we consider all funding from NIH as well as funding patterns globally, leveraging a database that also includes funding from other government agencies, national research councils, and foundations. Third, we utilize a more exhaustive set of search strings, coupled with a deeper analysis of the thematic categories of funded projects (see Supplementary Tables 1 and 2 for more details). We aim to offer timely insights into global funding for climate change and human health and have salient implications for setting future priorities for public and private investments in research.
To make the case that climate change deserves sustained and prioritized funding from the health sciences, health economics, implementation sciences, environmental health, and public health communities, consider that climate change can affect human health in ways as sobering as they are complex. Climate change can result in exposure to extreme heat of increasing severity and frequency, aggravated exposure to floods and droughts, and changes in the distribution of vector-borne diseases 21 . Risks and causal pathways between climate change and health can be direct and primary, such as temperature-enhanced levels of urban air pollutants, but also secondary and less direct, such as changes in water availability or food yields, or even tertiary and diffuse, such as mental health problems among suffering farming communities or refugees displaced by rising sea levels 22 .
Communicable and noncommunicable diseases associated with climate exposures represent a growing proportion of the overall morbidity and mortality risks 23 . A systematic review of the global impacts of ten climatic hazards linked to both greenhouse gas emissions and known human pathogenic diseases suggested that 58% (218 out of 375) of infectious diseases confronted by humanity worldwide have been at some point aggravated by climatic hazards 24 . Soberingly, the empirical cases analyzed by the review revealed 1,006 unique pathways in which climatic hazards, via different transmission types, led to pathogenic diseases. It concluded that “the human pathogenic diseases and transmission pathways aggravated by climatic hazards are too numerous for comprehensive societal adaptations,” 24 which in simple terms implies that the spread of climate change-induced diseases will far exceed our capacity to adapt or respond to them.
Recent analysis from the National Institutes of Health (NIH), an agency of the U.S. Department of Health and Human Services with 27 institutes and centers, similarly confirms the multidimensional relationship of climate change to human health, concluding in its Strategic Framework that “climate drivers affect health outcomes directly through weather events such as extreme heat, wildfires, droughts, storm surges, and floods, but also indirectly through a series of exposure pathways such as air and water quality, food quality, infectious diseases, and massive population displacement events.” 25 The NIH cautions that climate change significantly aggravates the risk of a long list of illnesses or injuries from asthma and allergies to waterborne and zoonotic diseases and that particular populations are disproportionately harmed, notably children, older adults, women and pregnant women, and persons with disabilities, as well as communities of color and rural populations 25 . Similarly, the most recent Assessment Report from the Intergovernmental Panel on Climate Change (IPCC) featured multiple chapters detailing the links between climate change and human health and wellbeing 26 .
As Fig. 1 summarizes, from 1985 to 2022, 0.26% of grant funding reported to NIH contained keywords related to climate change. During this period, the NIH funded more than two million projects (2,361,684), of which only 6,130 were related to climate change. Total project funding from the NIH from a more recent sample of projects from 2000 to 2022 involved about $ 620 billion ($619,691,645,384), about $ 2.2 billion ($2,209,643,448) or 0.36% of which went to climate change projects. In 2022, the most recent year in our analyses, climate change and health projects received about $ 281 million in total funding or 0.67% of total annual funding.
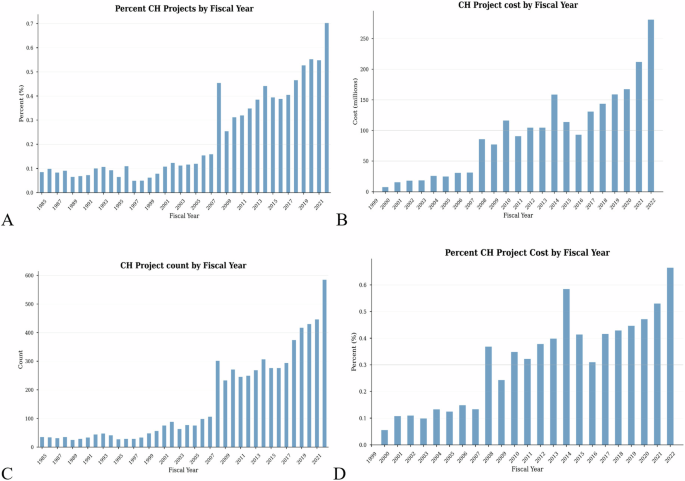
The above estimate for 2022 is similar to NIH’s own estimate of $ 293 million in funding for that year reported under the category of “Climate-Related Exposures and Conditions” 27 . However, examination of the grants included suggests that this definition of which funds are allocated to climate and health may overestimate the agency’s investments in this area. For comparison, the NIH also reports funding allocated in 2022 to “Climate Change” using a much more specific definition (albeit, less sensitive) of only $33 million. Although the estimated level of funding varies substantially depending on the definition of climate and health used, even the largest estimates still represent a tiny fraction of total NIH extramural research funding.
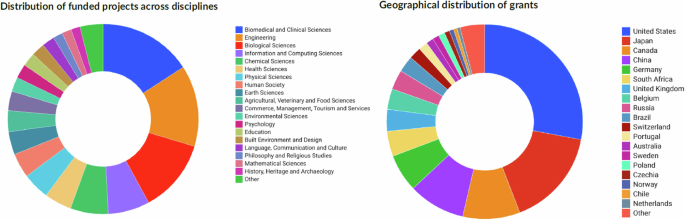
As depicted in Fig. 2, between 1985 and 2022 only 0.70% of funded projects in the Dimensions database related to climate change and human health—or 43,146 out of a total of 6,265,486 projects. In the more recent period from 2000 to 2022, Dimensions covered $ 1.943 trillion in funded projects, $ 20.928 billion or 1.1% of which was disbursed for projects identified as related to climate change and health. For 2022, the most recent year for which we have data, 1% of the annual count of grants and 1.83% of the total budgets of projects in the Dimensions database involved climate change and human health.
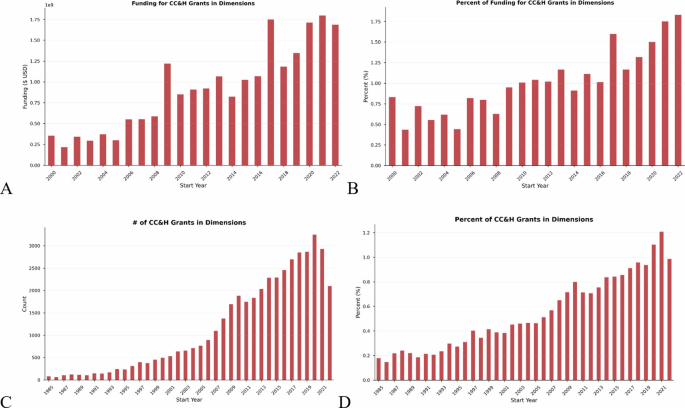
Figure 3 presents a graphic developed by the National Institute of Environmental Health Sciences (NIEHS, an institute within NIH) to illustrate some of the many interrelated issues with relevance to climate change and health research. The figure illustrates that changes in climate encompass aspects such as rising temperatures, sea level rise, or extreme weather events. Effects of climate change include, for example, exposure to air and water pollution, heat stress, or changing disease vectors, exposures which in turn may lead to higher rates of heat related illnesses, injuries, and death. The category of “Interventions and Strategies” highlights the importance of human responses such as preparedness, community awareness, or education.
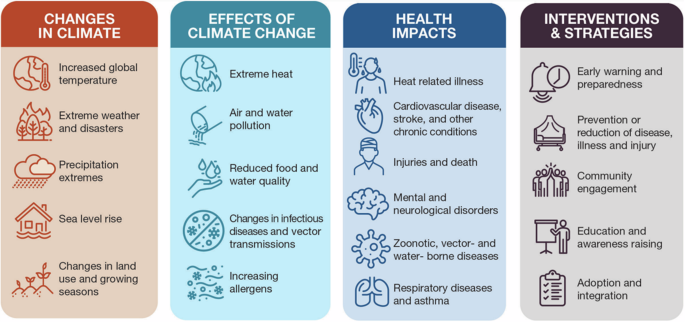
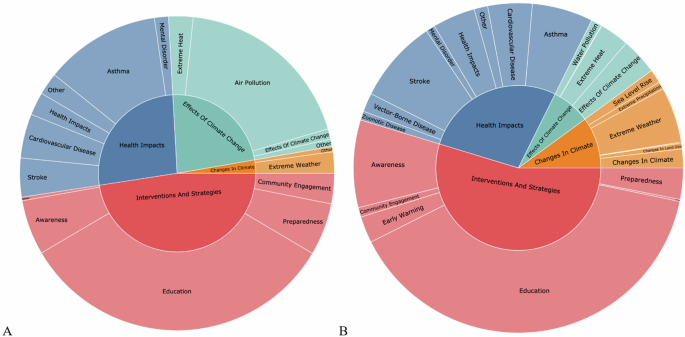
Figure 4 maps the funding patterns within the NIH RePORTER and Dimensions databases from 2000 to 2022 according to these four general thematic areas and 20 specific subcategories, with specific keywords described in Table 1 and Supplementary Table 5. Mapping is not mutually exclusive; projects can fall across multiple categories. Moreover, the use of this schematic and its categories is meant to provide an illustrative view of funding patterns across broad themes; we encourage researchers to consider other categorization rubrics building on this or other frameworks. Using this open approach, within NIH projects (Fig. 4A), the interventions and strategies area represent almost half of the funded projects within the sample, followed by health impacts and the effects of climate change, with the least funding disbursed to the areas of changes in climate. Interestingly, the same trend holds true for Dimensions projects (Fig. 4B).
We searched the Dimensions database for climate change and health grants (“records” within Dimensions) using similar search strings to the NIH RePORTER with the addition of General Disease terms, with Supplementary Table 2 offering a summary of our approach. Climate keywords used to query the Dimensions database were also matched to the Climate Change terms, and Climate Change Proxy terms from the NIH Climate Change and Health Literature Portal Search Strategy terms. The Climate and Health keywords were searched within the “full text” of each document (including title, abstract, full grant text when available, as well as other data fields included in the documentation) using the start year of the grant, between 1985 to 2022. Our analysis consists of collecting the annual grant count and funding to compare with the total collection of grants located in the Dimensions database.
Our approach has several important limitations. We searched only for information and projects available in English, meaning we likely overrepresented projects in the Global North in our dataset, although the Dimensions database does include projects in some country specific languages. We built our dataset by searching only the NIH RePORTER and Dimensions databases. We would not capture the extent of all research or funding connecting climate change with health, only those reported to the NIH or Dimensions Databases. In simpler words: we would have missed any projects not captured by these databases. Moreover, the NIH RePORTER database does not always reflect synergistic initiatives with other US federal agencies such as the EPA, NSF, CDC, NOAA, and NASA, which is why we coupled our analysis with the Dimensions database, which does cover those sources. Lastly, given that we harvested information via investigator reported abstracts (for NIH) and official research council or foundation records (for Dimensions), it is possible that certain terms or key words that were perceived to be controversial were removed or avoided (e.g., in Canada 34 and the United States 35,36 ). In those university cultures, some scientists across disciplines might feel compelled to minimize the visibility of the fact that their work very much informs climate questions, for all sorts of political or other reasons.
Furthermore, we may overestimate the volume of climate change and human health funding given that some of the titles or abstracts we searched may use words like “climate” or “heat”, but not always in the context of a project about climate change. Similarly, we included many terms for “weather” in our search strings (see Supplementary Tables 1-4) meaning we would capture some projects that deal only with weather events, but not necessarily those caused by or correlated with a changing climate.
Additionally, the NIH RePORTER query search is constrained by the generalization of climate terms used and the assumption all projects are related to human health, therefore animal studies may be included. The NIH RePORTER database did not allow us to search for truncations of the terms selected, limiting our detection of modified terminology. Our initial results for this perspective allow for a generalized conclusion about Climate and Health projects within the NIH RePORTER database. While the search query for the Dimensions database did allow for a truncation search, our scope was similarly limited due to the number of generalized health terms we included in our query, which did not include detailed exposure or disease terminology.
Lastly, in Fig. 4 and Table 1 we map funding patterns and results thematically using a framework developed by the National Institute of Environmental Health Sciences (NIEHS, an institute within NIH) to illustrate some of the many interrelated issues with relevance to climate change and health research. We acknowledge that this framework, although convenient and widely cited, was developed primarily as an illustrative tool rather than a prescriptive catalog of terms, does not provide an exhaustive list of disease or health impacts, combines education and awareness, and is limited to only a few categories.
We therefore fully acknowledge these results might be approximate due to the limited search terms used and the initial assortment of Climate and Health projects detected within the databases. We plan to execute a more in-depth query and analysis for a future publication (and encourage others to do so) that will expand on search terminology for both Climate and Health. We also call on future research to better differentiate between climate and weather and to discuss and analyze results that go beyond NIH’s Climate Change and Health Initiative framework.
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
The research reported in this publication was supported by the National Institute Of Environmental Health Sciences of the National Institutes of Health under Award Number U24ES035309. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.